Asherman's Syndrome - How Does It Affect Female Fertility?
Fertility Treatment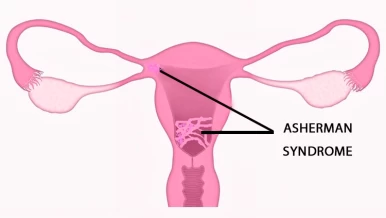
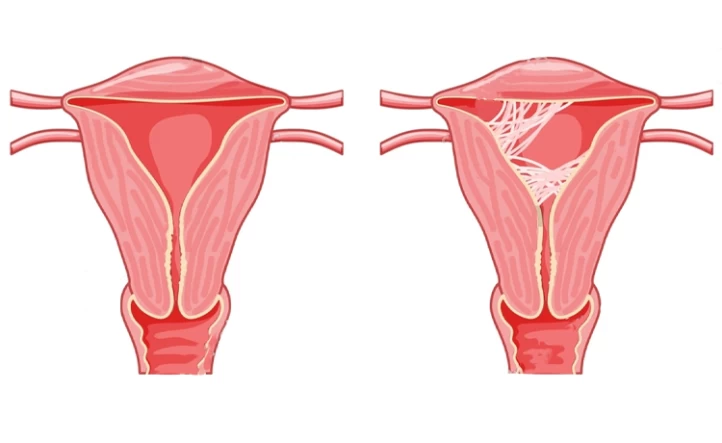
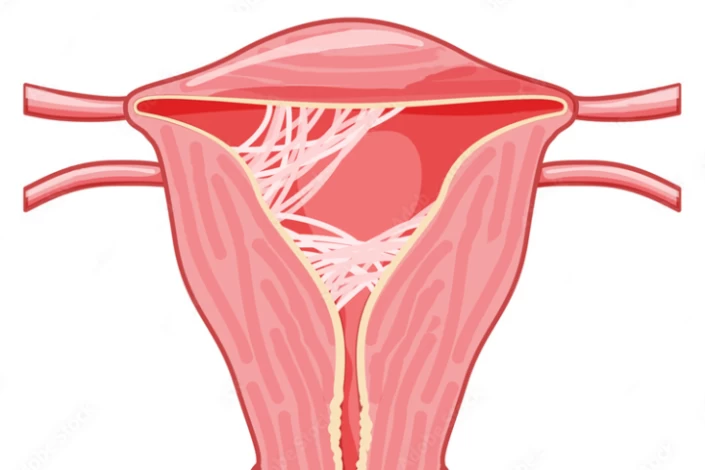
Intrauterine adhesion, also known as Asherman syndrome, is a condition characterized by the formation of scar tissue within the uterine cavity. This scar tissue can result from several factors, such as previous uterine surgeries, infections, or trauma to the uterine lining. As a result, the normal architecture of the uterus is disrupted, leading to potential complications such as abnormal uterine bleeding, recurrent miscarriages, and female infertility. Asherman syndrome symptoms include these complications.
The presence of intrauterine adhesions can significantly affect female fertility by altering the ability of the uterus to support a healthy pregnancy. The scar tissue can interfere with the implantation of a fertilized egg, leading to recurrent miscarriages or failed pregnancies. Furthermore, the intrauterine adhesions can obstruct the fallopian tubes or prevent the proper development of the endometrium, further compromising fertility. Asherman syndrome treatment often involves surgical intervention to remove the adhesions and restore normal uterine function.
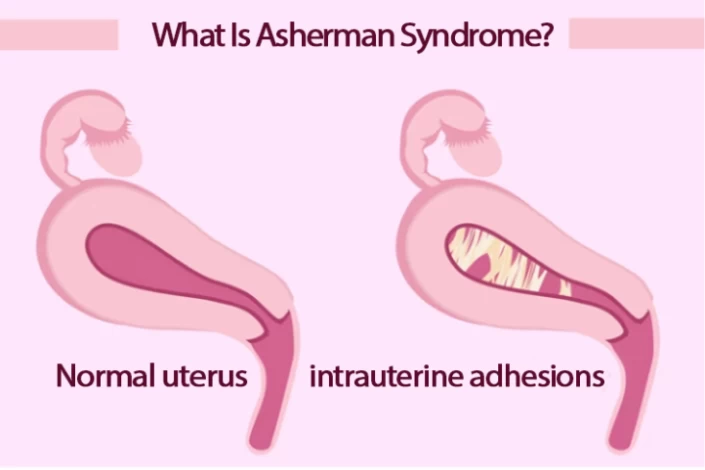
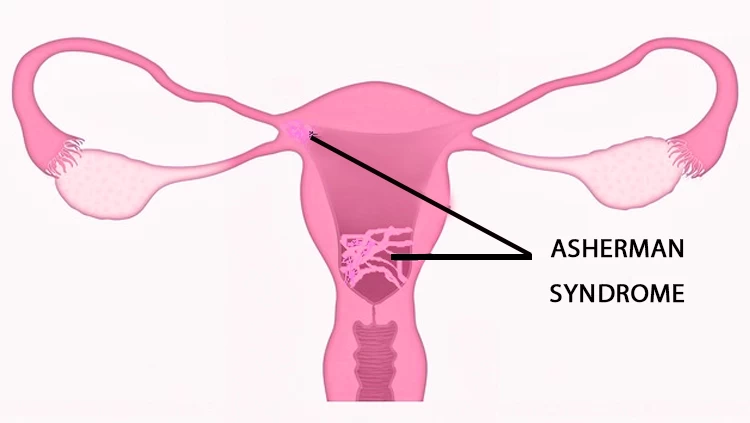
What Is Asherman Syndrome?
Asherman's Syndrome, also known as intrauterine adhesions, is a condition in which scar tissue forms inside the uterine cavity. This scar tissue can cause the walls of the uterus to stick together, leading to a variety of symptoms, including female infertility, irregular or absent menstrual periods, and recurrent miscarriages. Asherman syndrome can be caused by uterine surgeries such as dilation and curettage (D&C), cesarean sections, or myomectomy, as well as infections or inflammation of the uterus.
Women with Asherman's Syndrome may experience symptoms such as reduced menstrual flow, pelvic pain, and recurrent abortion. The presence of intrauterine adhesions can also impact fertility by interfering with the implantation of a fertilized egg, obstructing the fallopian tubes, or preventing the proper development of the endometrium. What causes Asherman's syndrome? It can result from various factors including surgical procedures on the uterus, infections, or severe inflammation.
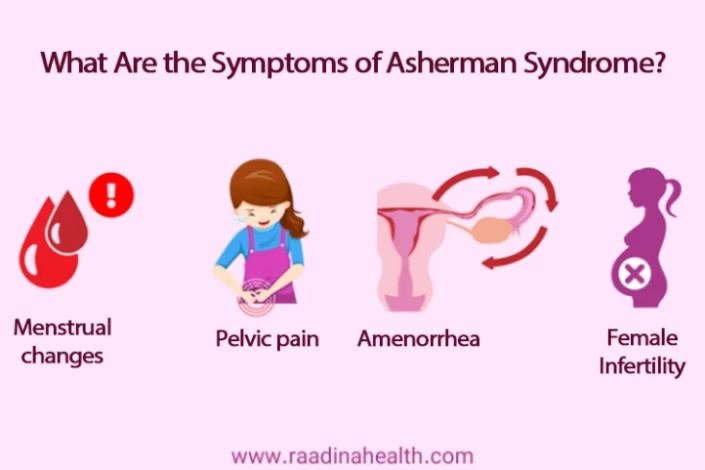
What Are the Symptoms of Asherman Syndrome?
The symptoms of Asherman's Syndrome can vary depending on the severity of uterine scarring and adhesions. Some common Asherman syndrome symptoms may include:
- Menstrual changes: Women with Asherman's Syndrome may experience changes in their menstrual cycle, such as lighter or absent periods (hypomenorrhea), irregular bleeding, or spotting between periods;
- Female Infertility: Asherman's Syndrome can cause scarring and adhesions in the uterus, which may lead to difficulty in conceiving or recurrent miscarriages. Women with the condition may have trouble getting pregnant or maintaining a pregnancy;
- Pelvic pain: Some women with Asherman syndrome may experience pelvic pain, especially during menstruation or sexual intercourse;
- Recurrent miscarriages: Asherman's Syndrome can increase the risk of recurrent miscarriages due to the presence of scar tissue in the uterus, which can affect implantation and the development of the fetus;
- Amenorrhea: In severe cases of Asherman's Syndrome, women may develop amenorrhea, which is the absence of menstrual periods.
How Is Asherman's Syndrome Diagnosed?
Asherman syndrome diagnosis is typically conducted through a combination of medical history, symptoms, and imaging studies. A gynecologist may begin the diagnostic process by taking a detailed medical history, including a discussion of the patient's menstrual history and any recent surgeries or procedures that may have affected the uterus. A pelvic examination may also be performed to assess the condition of the uterus and cervix. Your doctor may look for signs of scarring or adhesions inside the uterus.
Moreover, imaging tests such as hysterosalpingography (HSG) or transvaginal ultrasound may be used to visualize the inside of the uterus and assess for any abnormalities.
HSG involves injecting a contrast dye into the uterus and fallopian tubes while taking X-ray images. HSG can help visualize the shape of the uterine cavity and detect any blockages or abnormalities caused by Asherman's Syndrome. Transvaginal ultrasound uses sound waves to create images of the uterus and may reveal abnormalities such as uterine adhesions or irregularities in the endometrial lining.
A hysteroscopy may also be performed to directly visualize the inside of the uterus using a thin, flexible tube with a camera attached. This allows for a more detailed examination of the uterine cavity and any adhesions or scarring that may be present.

In some cases, a sonohysterogram (or saline infusion sonogram (SIS)) can be used to diagnose Asherman syndrome. This test involves injecting a sterile saline solution into the uterus during an ultrasound scan. The saline helps create a clearer image of the uterine cavity, making it easier to detect abnormalities like adhesions.
Based on the findings from these diagnostic tests, the gynecologist can confirm the presence of Asherman's Syndrome and determine the severity of uterine scarring.
How Is Asherman Syndrome Treated?
Asherman syndrome treatment typically involves a combination of surgical and non-surgical approaches, depending on the severity of the condition.
Here are some common Asherman syndrome treatment options for intrauterine adhesions:
- Hysteroscopic Surgery
- Hormone Therapy
- Intrauterine Balloon Therapy
- Adhesion Barriers
- Types of Infertility Treatments

Hysteroscopic Surgery
Once Asherman's Syndrome is diagnosed, hysteroscopic surgery can be used as a therapeutic intervention to treat the condition. During the procedure, specialized instruments are inserted through the hysteroscope to remove scar tissue, adhesions, or other abnormalities in the uterine cavity. This targeted approach helps restore normal uterine anatomy and function, improving menstrual cycles, fertility, and pregnancy outcomes for women affected by Asherman's Syndrome.
Hysteroscopic surgery for Asherman's Syndrome is typically performed on an outpatient basis, allowing patients to return home the same day as the procedure. Local anesthesia or sedation is commonly used to minimize discomfort during the surgery. Most women can resume normal activities within a day or two after hysteroscopy, with mild cramping, spotting, or light bleeding being common but temporary postoperative symptoms.
Hormone Therapy
Hormone therapy is often used as part of the treatment plan for Asherman's Syndrome to help promote the regrowth of healthy endometrial tissue and prevent the reformation of scar tissue in the uterus. Hormones such as estrogen and progesterone may be used to stimulate the growth of the uterine lining. Estrogen helps promote the regeneration of healthy tissue in the uterus, which is essential for restoring normal menstrual cycles and fertility. Progesterone helps support the growth and maintenance of the uterine lining, preparing it for the potential implantation of a fertilized egg.
Intrauterine Balloon Therapy
In some cases, a balloon catheter may be placed in the uterus after surgery to prevent the reformation of scar tissue and promote healing of the uterine lining. The balloon is typically left in place for a few days to weeks to allow for proper healing.
Adhesion Barriers
In more severe cases of Asherman's Syndrome, adhesion barriers may be used during surgery to prevent scar tissue from reforming. These barriers act as a physical barrier between the walls of the uterus, reducing the risk of adhesion recurrence.
Infertility Treatments
Assisted reproductive technologies (ART), such as in vitro fertilization (IVF), may be recommended for women with Asherman's Syndrome who have difficulty conceiving naturally to increase the chances of a successful pregnancy.
IVF treatment involves fertilizing eggs with sperm outside the body and transferring resulting embryos into the uterus for implantation. By bypassing potential barriers in the fallopian tubes or uterine cavity, IVF can help women with Asherman's Syndrome achieve pregnancy despite underlying infertility problems.
What Causes Uterus Scarring?
Asherman's Syndrome is typically caused by damage to the lining of the uterus (endometrium) following certain gynecological procedures or conditions. Asherman syndrome cause can include uterine surgeries such as::
- Dilatation and curettage (D&C): A D&C procedure involves scraping or suctioning the lining of the uterus, often performed after a miscarriage, abortion, or to diagnose or treat certain gynecological conditions. If not performed carefully, it can lead to scarring and adhesions in the uterus.
- Cesarean section (c-section): Any surgery involving the uterus, such as a cesarean section, can increase the risk of developing Asherman's Syndrome due to potential damage to the endometrium.
- Infections: Infections of the uterus, such as endometritis (inflammation of the endometrium) following childbirth, miscarriage, or other gynecological procedures, can lead to scarring and adhesions.
- Radiation therapy: Radiation treatment for certain cancers in the pelvic area, like cervical cancer, can damage the endometrium and lead to the formation of scar tissue in the uterus.
Can Asherman's Syndrome Cause Female Infertility?
As mentioned earlier, Asherman's Syndrome is a condition in which scar tissue forms inside the uterus, typically as a result of uterine surgery or infection. This scar tissue, or intrauterine adhesions, can cause the walls of the uterus to stick together or become wholly or partially blocked. As a result, the endometrium, the lining of the uterus where a fertilized egg would implant and grow, may not be able to develop properly. This can lead to irregular or absent menstrual cycles, as well as difficulty in achieving and maintaining a pregnancy.
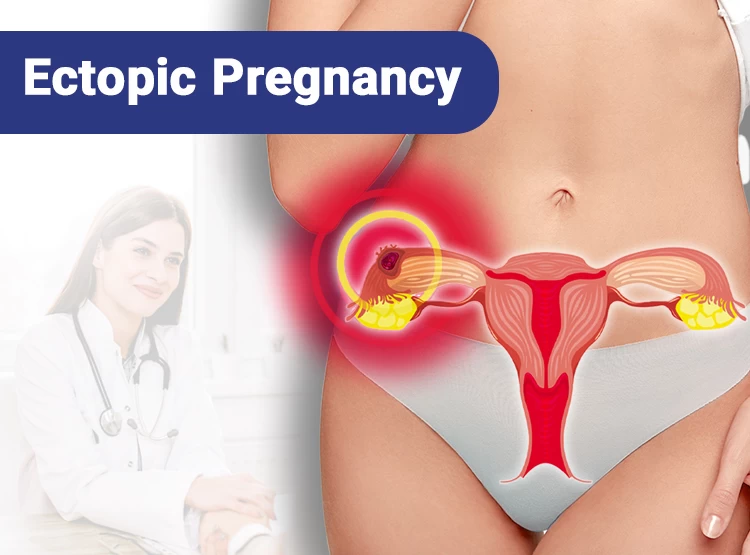
In addition to affecting the endometrium, Asherman's Syndrome can also interfere with the ability of the fallopian tubes to transport a fertilized egg to the uterus. If the scar tissue blocks the entrance of the tubes or impairs their function, this can prevent the egg from reaching the uterus and result in female infertility. Furthermore, the scarring may also affect the overall structure of the uterus, making it difficult for an embryo to implant and grow.
However, with proper diagnosis and treatment, including surgical removal of adhesions, hormonal therapy to support endometrial regeneration, and assisted reproductive technologies (ART) like IVF, most women with Asherman's Syndrome can improve their chances of conceiving and carrying a pregnancy.
Can Asherman Syndrome Cause Miscarriage?
Asherman Syndrome can cause miscarriage by creating scar tissue within the uterus that can interfere with the implantation of a fertilized egg. The scar tissue, or intrauterine adhesions, can disrupt the normal functioning of the uterus and prevent a pregnancy from developing correctly. This can lead to a higher risk of miscarriage as the embryo may not be able to implant or grow as it should.
Additionally, Asherman Syndrome can cause issues with the blood supply to the uterus, leading to a decrease in the supply of oxygen and nutrients to the developing fetus. This can result in a miscarriage as the embryo may not receive the necessary support to grow and develop properly. The scarring from Asherman Syndrome can also affect the thickness of the uterine lining, which is essential for a healthy pregnancy.
How Common Is Asherman Syndrome?
The exact prevalence of Asherman's Syndrome is not well-established, as it can be underdiagnosed or misdiagnosed in some cases. However, it is generally considered to be a relatively rare condition. Asherman's Syndrome is more commonly seen in women who have undergone multiple dilatation and curettage (D&C) procedures, particularly after a miscarriage or termination of pregnancy.
Can Asherman Syndrome Be Prevented?
While it may not always be possible to prevent Asherman's Syndrome, taking proactive steps to protect uterine health and minimize potential risk factors can help reduce the likelihood of developing this condition. By maintaining open communication with your doctor, seeking prompt treatment for uterine issues, and following recommended guidelines for postoperative care, women can take proactive measures to safeguard their reproductive health and reduce the risk of developing Asherman's Syndrome.
Infertility Treatment in Iran
Infertility treatment in Iran has seen significant advancements in recent years, making it a popular destination for individuals seeking fertility treatments. The country offers a wide range of infertility treatment options, including in vitro fertilization (IVF), intrauterine insemination (IUI), and egg donation.
One of the main reasons for the popularity of infertility treatment in Iran is the high success rates and affordable prices compared to other countries. Many couples from neighbouring countries choose Iran for their fertility treatments due to the quality of care and expertise of medical professionals.
Iran also boasts a large number of fertility clinics and hospitals that specialize in Types of Infertility Treatments, equipped with state-of-the-art facilities and advanced technology. This has helped the country establish itself as a leading destination for infertility treatment in the region.
Furthermore, the supportive and compassionate approach of Iranian medical professionals towards patients undergoing infertility treatment is highly appreciated by those seeking help in conceiving. The doctors and staff at these fertility clinics make sure to provide personalized care and emotional support to patients throughout the treatment process.

FAQs About Asherman's Syndrome
1) Can an IUD cause Asherman's Syndrome?
Asherman syndrome is typically caused by injury or trauma to the uterine lining, such as from a prior uterine surgery or infection. There is no evidence to suggest that an IUD can cause Asherman's Syndrome.
2) Can I get pregnant after being treated for Asherman's Syndrome?
Many women with Asherman's Syndrome can conceive after successful treatment to remove the adhesions and restore normal uterine function. However, the severity of the scarring and any underlying fertility issues can impact fertility outcomes. In some cases, assisted reproductive technologies such as in vitro fertilization (IVF) may be recommended to help achieve pregnancy.
3) Can Asherman's Syndrome be cured?
If your treatment for Asherman's Syndrome is effective, you can expect an improvement in your symptoms. Your doctor will continue to assess your condition to ensure that no new scar tissue forms.
4) Is Asherman's Syndrome genetic?
Asherman's Syndrome is not considered to be a genetic condition. It is typically caused by scarring and adhesions in the uterus that may develop as a result of damage to the uterine lining, often from procedures such as dilation and curettage (D&C) or infections following childbirth or miscarriage. Genetic factors do not play a significant role in the development of Asherman's Syndrome.
5) Can Asherman's Syndrome recur after treatment?
Asherman's Syndrome can recur after treatment, especially if the underlying cause of the condition is not addressed or if there is repeated trauma to the uterus.
6) Are there any long-term complications associated with Asherman's Syndrome?
Left untreated, Asherman's Syndrome can lead to infertility, recurrent miscarriages, and complications during pregnancy, such as placental abnormalities or preterm labour.
7) Can Asherman's Syndrome affect menstrual cycles?
Asherman's Syndrome can cause changes in menstrual cycles, such as lighter or absent periods, irregular bleeding, or painful periods. Hormone therapy may be recommended to help regulate the menstrual cycle.
8) Can endometriosis cause Asherman's Syndrome?
Endometriosis is an inflammatory condition that can result in the inability to shed the tissue lining of the uterus properly. This can, in turn, cause Asherman's Syndrome.













No reviews
Your comment