Uterine Polyps: Can It Cause Infertility or Miscarriage?
Fertility Treatment
Pregnancy is an extraordinary journey filled with joy, anticipation, and countless emotions. However, for some women, this excitement can be overshadowed by concerns surrounding their reproductive health, including the development of polyps in the uterus. One such concern that deserves attention is the presence of uterine polyps. This often misunderstood condition can potentially impact a woman's ability to conceive and carry a pregnancy to term.
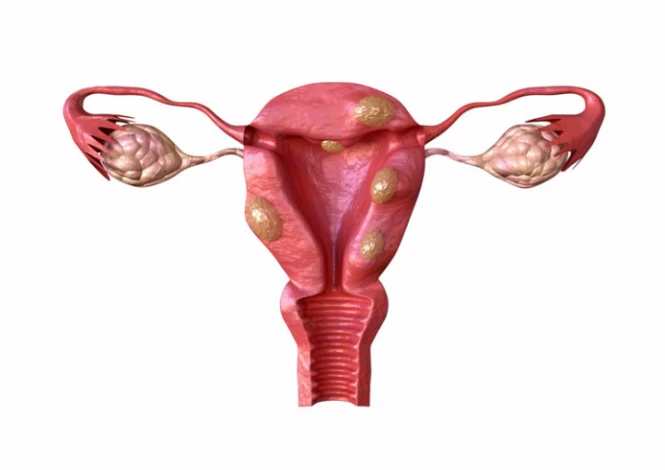
A uterine polyp, also known as an endometrial polyp, is a growth that develops in the inner lining of the uterus (the endometrium). These polyps are typically non-cancerous, but some have the potential to develop into precancerous polyps.
Although uterine polyps are more common in women who are going through menopause, they occasionally can be seen in younger women. Recognizing symptoms of polyps in the uterus, such as abnormal bleeding or pelvic pain, is crucial in seeking timely medical attention. Understanding how to prevent polyps in the uterus and knowing the available diagnostic methods and treatment for uterine polyps are essential for maintaining reproductive health and ensuring a smooth pregnancy journey. Additionally, addressing the question "Can polyps cause infertility?" is important, as these growths can sometimes impact fertility, though not always.
This article will explore the characteristics of uterine or endometrial polyps, including their symptoms, causes, diagnostic methods, and treatment options.

What Is a Uterine Polyp?
A uterine polyp is a small growth that develops on the inner lining of the uterus (endometrium). They can occur in women of any age but are more common in women who have gone through menopause. Uterine polyps can vary in shape (round or oval) and size, ranging from a few millimeters (the size of a sesame seed) to a few centimeters (the size of a golf ball).
Endometrial polyps are attached to the endometrium by a thin stalk or a broad base. However, if they overgrow, they can enter the vagina and increase the risk of cervical cancer and pregnancy disorders.
Can uterine polyps cause infertility?
Uterine polyps can cause infertility in some cases. This is because they can interfere with the implantation of a fertilized egg in the uterus. The polyps can also affect the shape and size of the uterus, making it difficult for a fertilized egg to attach and grow properly. Additionally, polyps in the uterus can cause abnormal bleeding, which can make it difficult to time ovulation and conceive. However, not all women with uterine polyps experience infertility.
Contact us for a free initial consultation about uterine polyps.
WhatsAppTelegramFacebookEmailHow Do Polyps in the Uterus Lining Affect Pregnancy?
The size of uterine polyps is typically small, about a few millimeters. Therefore, they may not much affect pregnancy. However, if the endometrial polyps become large, they can disrupt the natural structure of the endometrium of the uterus, making embryo implantation and pregnancy with uterine polyps difficult. In such a situation, the risk of mischarges may increase.
Cervical polyps are common in women who have given birth more than once and do not have any specific symptoms in most cases. Therefore, if cervical polyps are small and few, they do not pose a threat to the health of the mother or the fetus. However, if multiple polyps are growing in the cervix, it can increase the risk of frequent infections, heavy bleeding during childbirth, or premature birth.
In severe cases where uterine polyps affect fertility by hindering embryo implantation, the risk of miscarriage may increase. Therefore, it's essential for individuals experiencing symptoms or concerned about uterine polyps to seek medical evaluation and appropriate treatment to optimize reproductive health and increase the chances of a successful pregnancy.
What Are the Symptoms of Uterine Polyps in Non-Pregnant Women?
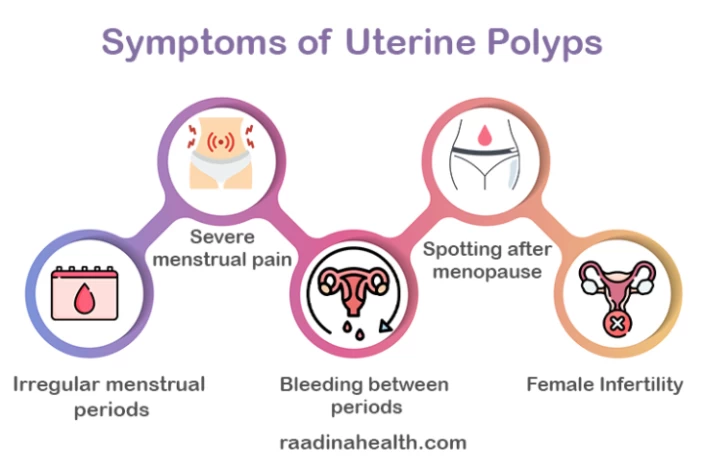
Some of the most common symptoms of polyps in the uterus include:
- Irregular menstrual periods;
- Severe menstrual pain;
- Heavy and abnormal menstrual bleeding;
- Bleeding between periods;
- Spotting after menopause;
- Bleeding after intercourse;
- Female Infertility.
It is important to note that not all women with uterine polyps will experience symptoms. Some women may only discover they have polyps during a routine pelvic exam or ultrasound.
What Are the Symptoms of Uterine Polyps in Pregnant Women?
Symptoms of uterine polyps in pregnant women can include frequent vaginal infections and foul-smelling or pus-like white or yellow vaginal discharge (due to infection). In such cases, seeing a doctor for necessary examinations is necessary.
What Causes Uterine Polyps?
Risk factors that may increase the risk of uterine polyps can be as follows:
- Hormonal disorders, especially an imbalance in estrogen hormone levels;
- Age - Endometrial polyps are more common in women aged 40 to 50 years and are rarely seen in younger women of 20 years or less;
- Obesity;
- High blood pressure;
- Polycystic Ovary Syndrome (PCOS) due to high levels of estrogen;
- Family history;
- Previous uterine surgery;
- Use of tamoxifen is a medication used to treat breast cancer.
How to Diagnose Uterine Polyps?
Doctors used to remove undiagnosed uterine polyps during Dilation and curettage (D&C) procedures in the past. This could help treat infertility in couples with unexplained infertility. Nowadays, doctors use hysteroscopy to visualize the uterine cavity and detect any polyps directly. Once diagnosed, the polyp is removed through hysteroscopy or other surgical methods.
Transvaginal ultrasound can also visualize the inside of the uterus and diagnose uterine polyps. This Imaging test is performed on days 10 to 12 of the menstrual cycle because endometrial thickness is at its greatest due to increased estrogen levels.
Therefore, if the ultrasound is performed at the wrong time of the menstrual cycle, the uterine polyp will not be easily diagnosed.
Other methods for diagnosing endometrial polyps include Sonosalpingography (SSG), the Sion test, Hysterosonography, and saline-infusion sonohysterography (SIS). During hysterosonography, a healthcare provider injects a saline solution into the uterus through a small catheter and then performs a transvaginal ultrasound to visualize the endometrial polyp, which is seen as a filling defect. However, the HSG method is not effective in detecting small polyps.

How to Treat Uterine Polyps?
According to research, small and asymptomatic polyps usually resolve on their own. However, these benign polyps can sometimes get malignant.
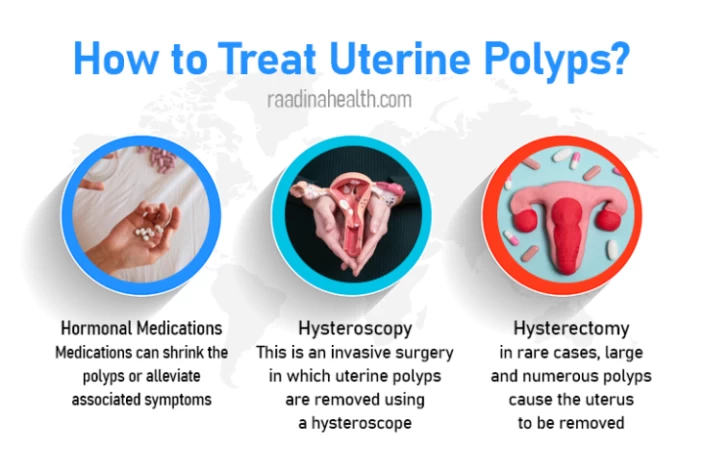
Treatment for uterine polyps might involve:
Medications
Medication cannot fully cure uterine polyps. However, hormonal medications, such as progestins or gonadotropin-releasing hormone agonists, can be prescribed to help shrink the polyps or alleviate associated symptoms. Obviously, in such cases, the condition will recur if the drug is stopped.
Hysteroscopic polypectomy
Hysteroscopic polypectomy is a minimally invasive surgical procedure in which uterine polyps are removed using a hysteroscope, which is a thin, flexible instrument that is inserted through the vagina and cervix into the uterus. The hysteroscope has a camera and a light on the end, which allows the doctor to see inside the uterus and locate the polyps.
Once the polyps are located, the doctor removes them using small instruments. These may include a loop electrode or a curette, which are used to cut the polyp away from the uterine wall. The removed tissue is then examined in a lab to ensure it is not cancerous.
Hysterectomy
The doctor may recommend a hysterectomy in rare cases where the polyps are large, numerous, or causing severe symptoms. Hysterectomy is a surgical procedure in which the uterus is removed.
How Is Recovery from Endometrial Polyp Removal?
Patients may have some discomfort and tenderness after the polypectomy procedure. The doctor will prescribe pain medication to soothe this period-like pain.
Patients may have light bleeding immediately after a uterine polyp removal. They may also be discharged for up to 14 days after the treatment. The fluid may be light pink to brown.
The menstruation cycle will return to normal after a polypectomy, while a hysterectomy ends periods because it removes the entire uterus.
This may take about two weeks to recover from a polypectomy. Recovery time for a hysterectomy takes four to six weeks or longer.
Recovery time also differs from person to person. Therefore, patients should consult their doctor a week after the procedure to determine when they can return to work and other activities.

Do All Uterine Polyps Need to be Removed?
The decision to remove uterine polyps depends on various factors, including the size and number of polyps, symptoms experienced by the individual, and whether there are concerns about cancer or infertility.
Large and numerous polyps with obvious symptoms must be removed in any condition at any age to prevent further complications.
Small and asymptomatic uterine polyps may not require treatment. However, asymptomatic polyps should be removed in the following situations:
- Female Infertility;
- Postmenopausal Bleeding
- Recurrent miscarriages;
- Numerous Polyps larger than 1.5 cm;
- Polyps hanging from the cervix.
What Is a Cervical Polyp?
A cervical polyp is a small, finger-like growth that develops on the cervix (a narrow passage that connects the uterus to the vagina). These polyps are usually non-cancerous and are typically about 1 to 2 centimeters in size. They can grow as singular or multiple masses and have smooth or irregular surfaces.
Studies have shown that cervical polyps are more common in women who have given birth to more than one child and those who are in their 40s and 50s. Also, higher estrogen levels may increase the risk of developing cervical polyps.
Cervical polyps are categorized depending on their origin: ectocervical and endocervical polyps. Ectocervical polyps, which arise from the outer surface layer of cells on the cervix, are more common in women who've gone through menopause. Endocervical polyps, which arise from the cervical glands in the endocervix, are more common and typically happen in premenopausal women. However, the likelihood of developing this condition in girls who haven't begun to menstruate is very low.
While cervical polyps themselves may not pose a direct threat to a successful pregnancy, multiple polyps or their associated symptoms, such as heavy bleeding, may warrant medical attention to optimize reproductive health and ensure a successful pregnancy with cervical polyps.
How to Prevent Polyps in Uterus?
Preventing polyps in the womb involves a combination of proactive measures and lifestyle choices:
- It's essential to prioritize regular gynecological check-ups and seek medical attention promptly if you experience any symptoms associated with uterine polyps, such as abnormal bleeding or pelvic pain.
- Proper hygiene is crucial; opting for breathable cotton underwear can help prevent moisture buildup and create an environment less conducive to infection growth. Practicing safe sex by using contraceptives like condoms not only reduces the risk of sexually transmitted infections but also minimizes the chance of developing uterine polyps linked to certain infections.
- Adopting a healthy lifestyle, with a balanced diet rich in fruits, vegetables, whole grains, and regular exercise, can contribute to overall reproductive health and potentially lower the risk of uterine polyps.
Always consult your healthcare provider for personalized advice and recommendations tailored to your needs and medical history.
Why Iran for Infertility Treatment?
Iran has become a popular destination for infertility treatment. The country has numerous specialized clinics and fertility centers offering state-of-the-art For a variety of infertility treatment methods equipment and technologies.
Iran boasts a pool of highly skilled and experienced infertility specialists. Many of these specialists have received training and education from top international institutes and are proficient in the latest techniques and procedures for infertility treatment.
Infertility treatments in Iran are generally more affordable compared to many other countries, especially in the Western world. This cost-effectiveness makes it an attractive option for couples seeking infertility treatment, particularly for those who may not have access to affordable treatment options in their home countries.

Final Word
Understanding the impact of a uterine polyp on pregnancy is crucial for women planning to conceive. A uterine polyp can disrupt the fertile environment within the uterus, hindering the implantation of fertilized eggs and increasing the risk of miscarriage. It can also lead to irregular menstrual cycles, abnormal bleeding, and fertility issues. However, through timely diagnosis and appropriate management, such as hysteroscopic polypectomy, women with uterine polyps can increase their chances of successful pregnancies.
Frequently Asked Questions on Uterine Polyps
1) Do uterine polyps cause miscarriage?
Experts believe that uterine polyps do not increase the risk of miscarriage on their own. However, women with recurrent miscarriages need to examine their uterine cavity using methods such as transvaginal ultrasound or color Doppler ultrasound. If uterine polyps are diagnosed, they should be removed immediately, preferably through Hysteroscopy, to prevent further complications.
2) Do Uterine Polyps Occur in Virgin Girls?
Many virgin girls may experience spotting or abnormal menstrual bleeding. However, it cannot be conclusively attributed to uterine polyps. This is because several conditions can affect the reproductive organs of women and young girls, and many of them have similar symptoms. Therefore, seeking medical attention and undergoing thorough examinations is advisable to determine the underlying cause.
3) Are uterine polyps associated with an increased risk of uterine cancer?
Uterine polyps are generally considered benign (non-cancerous) growths, and most of them do not increase the risk of uterine cancer. However, in rare cases, some types of polyps may be associated with an increased risk of developing uterine cancer. These polyps are usually larger, have abnormal cells, and are more common in postmenopausal women. Therefore, it is important to monitor any changes in symptoms or growth of uterine polyps and consult a doctor for appropriate evaluation and management. Regular gynecological exams and screenings can also help detect potential issues early on.
4) Are uterine polyps likely to reoccur after treatment?
There is a chance that uterine polyps may reoccur after treatment, but it depends on various factors such as the size and number of polyps, the underlying cause, and the type of treatment received. Factors like hormonal imbalances and certain medical conditions may increase the likelihood of polyps returning.
5) Can uterine polyps be detected through a routine pelvic exam?
Uterine polyps are typically not detectable through a routine pelvic exam alone. While a pelvic exam may reveal abnormalities or suggest further investigation, definitive diagnosis usually requires imaging tests like a transvaginal ultrasound or procedures such as hysteroscopy.
6) What is the role of hysteroscopy in managing uterine polyps?
Hysteroscopy is a key diagnostic and treatment tool for uterine polyps. It involves inserting a thin, lighted tube (hysteroscope) through the vagina and cervix to view the inside of the uterus. Polyps can be identified, biopsied, or removed during this procedure, depending on their size and symptoms.
7) Are there any lifestyle changes that can help manage uterine polyps?
While lifestyle changes cannot prevent uterine polyps, maintaining a healthy lifestyle can help manage symptoms and support overall reproductive health. This includes a balanced diet, regular exercise, healthy weight, and stress management.
8) How do uterine polyps affect menstrual cycles?
Uterine polyps can cause a variety of menstrual irregularities, including heavy menstrual bleeding, spotting between periods, and longer or more frequent periods. They may also contribute to cramping or pelvic pain.
9) Can uterine polyps affect hormone levels?
Uterine polyps themselves do not usually affect hormone levels directly. However, hormonal imbalances, particularly involving estrogen, are thought to contribute to the development of polyps. Managing hormone levels may help prevent or reduce the occurrence of polyps.













No reviews
Your comment